Referrals & Advocacy
As a primary care provider it is important to be an advocate for your patient and support them to actualizing their gender in all all areas of their life. Below are resources that help you and your patient in navigating systemic barriers in health and legal and policy.
Changing sex designation
-
Template Letter in Support of an Application For Change of Sex Designation on an Ontario Birth Registration
-
Template Letter in Support of an Application For Change of Sex Designation on an Ontario Driver’s License
Support Letters
Inquiring around how transitioning may influence the vocational or educational situation of the patient is important, as providers can help the patient develop strategies for dealing with gender transition in school or the workplace. Unfortunately it is not uncommon for transition to result in the loss of a job or struggle in academic setting.
Sample Support Letter for Trans Patients Applying for EI through the Just Cause Mechanism
Submit Exceptional Access Program (EAP) form for patients on Ontario Drug Benefit (ODB)
Patients covered by the Ontario Drug Benefit (ODB) program include those on Ontario Works (OW), the Ontario Disability Support Program (ODSP), seniors ≥65 years of age, youth ≤24 years of age without private insurance (via OHIP+) and those on the Trillium Drug Program. For patients on ODB, injectable testosterone is covered with the submission of an Exceptional Access Form (EAP), while anti-androgens and estradiol are covered without the need for EAP approval.
Recommendation: Injectable testosterone is funded by the Ontario Drug Benefit (ODB) program for gender affirmation with an Exceptional Access Program (EAP) request. We suggest that providers submit EAP requests for both testosterone cypionate and testosterone enanthate, so that delays in access do not result when one formulation is on back order or not locally available. (See Appendices N and O in the Guidelines for samples).
-
Sample Request for an Unlisted Drug Product, Testosterone Enanthate (Delatestryl)
-
Sample Request for an Unlisted Drug Product, Testosterone Cypionate (Depo-Testosterone)
Overview of Ontario Process for Transition-related surgery (TRS)
This section provides a brief overview of the Ontario system for TRS planning visit(s) and referral. It is not exhaustive nor intended as training for conducting TRS planning visits.
Since TRS was relisted under OHIP coverage in 2008, surgical referral was delegated solely to the CAMH Adult Gender Identity Clinic. However in March 2016, the Ministry of Health and Long Term Care (MOHLTC) announced a regulatory change that allowed qualified providers outside of CAMH to conduct TRS Planning Visits and TRS referrals. This positive change has increased access to TRS for trans Ontarians and has encouraged a shift towards the provision of trans-related health care in the primary care setting.
Benefits of surgical referral coordination in primary care:
- Depathologizes gender diversity
- Recognizes the relationships that are built in primary care over time
- Allows for increased access, particularly for rural and remote trans patients with limited access to travel
Current MOHLTC-fundedi transition-related surgeries include:
| For patients assigned male at birth | For patients assigned female at birth | ||
|---|---|---|---|
| Upper body | Augmentation Mammoplastyii | Mastectomyiii | |
| Gonadal | Orchiectomy | Hysterectomy Salpingo-oophorectomy |
|
| External Genital | Vaginoplasty | Clitoral Release with vaginectomy Metoidioplasty Phalloplasty Testicular Implants with scrotoplasty Penile Implant |
|
|
|||
For more detailed information on individual transition-related surgeries, please download the RHO TRS Summary Sheets
Overview of the TRS planning and referral process
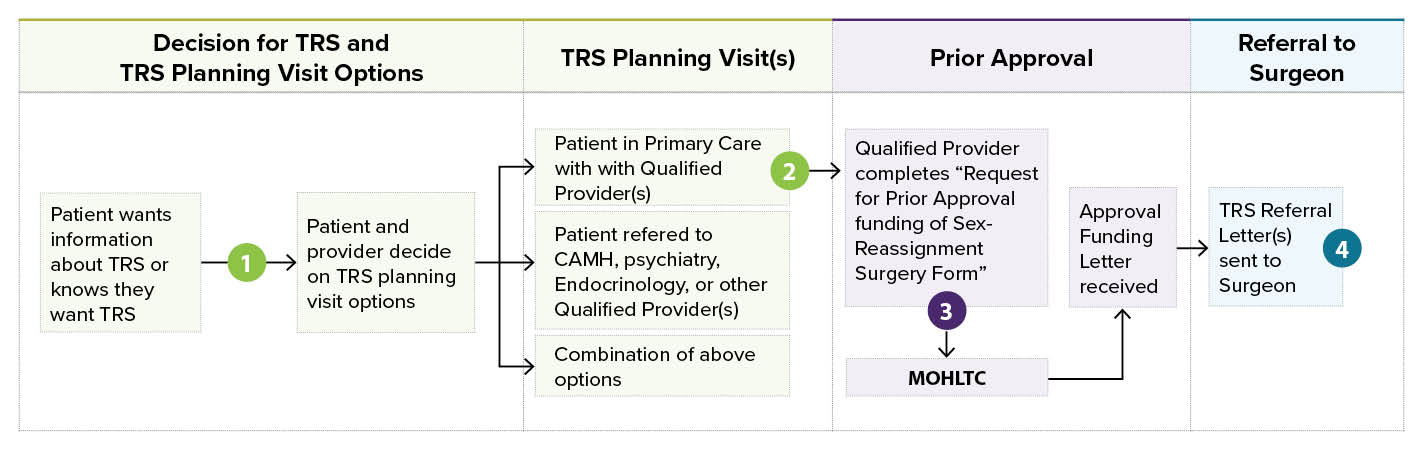
To learn more about each step, click on the numbers 1-4 below:
Decide which Qualified Provider(s)will conduct the TRS planning visit(s) and hence complete the MOHLTC Prior Approval from.
The MOHLTC requires the Prior Approval form to be completed by “a provider trained in the assessment, diagnosis and treatment of gender dysphoria in accordance with the World Professional Association for Transgender Health (WPATH) Standards of Care…”, and it is expected that the Qualified Provider who signs the Prior Approval form has conducted a complete TRS planning visit. Patients and their providers may choose what works best given individual patient needs and local resources.
Who is a Qualified Provider?
- The MOHLTC has maintained that providers should determine for themselves if TRS planning visits and referrals fall within their scope of practice, as providers would generally self-determine in other areas of care. There is no single training course that ‘qualifies’ a provider; rather a provider can become ‘qualified’ by any number of activities, including but not limited to: attending continuing medical education (CME) on trans surgical care through RHO, CPATH or WPATH; working at a health facility that practices trans primary care in accordance to WPATH guidelines; obtaining mentorship from an experienced colleague, through participation in the RHO trans mentorship call, or ECHO Ontario on Trans and Gender Diverse Healthcare. A provider who is new to this area of practice may want to combine a number of these activities to gain the necessary expertise.
Providers can gain TRS knowledge and access mentorship through:
- WPATH SOC
- RHO Workshops on Transition-related Surgeries
- RHO trans care mentorship call
- Sherbourne Health TRS Summary sheets (valuable resource to facilitate discussion between provider and patient)
- UofT/CAMH Trans ECHOR
- Trans E-consult, Champlain LHIN
- Mentorship with an experienced provider
A TRS planning visit is a collaborative visit between patient and a qualified provider to discuss TRS and how to optimize the patient’s experience and outcome. Topics discussed include WPATH and MOHLTC criteria, confirming the diagnosis of gender dysphoria, reviewing the stability of medical and mental health conditions, a surgery-specific informed consent discussion and aftercare planning.
All primary care providers can support patients during the TRS process, whether or not they conduct the TRS planning visit(s)
Whether a patient has TRS planning visits in Primary Care or with CAMH or another Qualified Provider, there are many ways that a primary care provider can support a patient throughout the TRS process. Providers can help prepare patients for surgery by assisting in the optimization of medical and mental health conditions, supporting smoking cessation, discussing the aftercare plan, preparing for travel, finances and supplies, and providing emotional support. Some patients may benefit from peer support and information such as that provided by Sherbourne Health’s Surgical Support Groups for Community Members.
View tips on how to support patients throughout the TRS process
Complete, sign, and submit the “Request for Prior Approval for Funding of Sex-Reassignment Surgery” (also known as the “Prior Approval” form) to the MOHLTC.
The number of qualified providers who must complete independent TRS surgery planning visits and sign a Prior Approval from is based on the type of surgery requested. Upper body surgery requires a TRS planning visit(s) by one qualified provider (either a physician or NP). Gonadal or external genital surgery requires independent TRS planning visits with two qualified providers, one of whom must be a physician or NP, while the second can be a physician, NP, registered nurse, psychologist, or a registered social worker with a Masters of Social Work. Only the Prior Approval form should be sent to the MOHLTC; TRS clinical notes and referral letters should not be sent. The MOHLTC will then send a response letter with the outcome of the funding application.
Once an Approved Funding Letter is received, the qualified provider(s) can then send TRS referral letters to the TRS surgeon. TRS referral letters are different from typical referral letters; they include a large amount of information regarding the topics covered in the TRS planning visits. Providers should be familiar with the WPATH recommendations for TRS referral letters. Most surgeons will require complete documentation of thorough TRS planning visit(s). Additional materials such as medication lists, lab results, ECG, and/or photographs may be required by some surgeons before an appointment is booked.
RHO's FAQson Transition-related surgery (TRS)